Abstract
Introduction: An increased risk of arteriosclerosis and cardiovascular disease has been noted in cancer survivors. However, there are only a few reports available that consider the risk of arteriosclerosis in patients treated with chemotherapy. R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone) regimen is a standard treatment for patients with B-cell malignant lymphoma. In this regimen, prednisolone has a potential risk of diabetes mellitus (DM), hyperlipidemia (HL), and osteoporosis and doxorubicin has cardiotoxicity. However, there are no studies that have investigated the effect of R-CHOP therapy on arteriosclerosis. An arterial stiffness parameter, the cardio-ankle vascular index (CAVI), was developed as a marker evaluating arteriosclerosis of aorta, femoral and tibial arteries. The principle of CAVI is based on the stiffness parameter ß theory proposed by Hayashi et al, and it is based on the variance of the arterial pressure that is required to change the vascular diameter. So, CAVI does not depend on blood pressure changes during the measurement. As previously demonstrated, CAVI is significantly elevated in arteriosclerotic diseases such as coronary artery disease and cerebral infarction. We reported the first report evaluating the changes of CAVI during R-CHOP therapy in a patient with follicular lymphoma (2017, J Clin Med Res.). The patients had an elevated CAVI in combination with plaque formation after 8 cycles of R-CHOP. In this study, we evaluated CAVI in patients with malignant lymphoma treated with R-CHOP therapy. In addition, we investigated the change of von Willebrand factor (vWF) as a vascular endothelial damage during the treatment.
Materials and methods:Patients with B cell malignant lymphoma who received R-CHOP therapy were enrolled from April 2014 to January 2017. The changes in CAVI before and after the first and the final courses of R-CHOP were evaluated. Some recent patients who did not complete R-CHOP therapy were also evaluated the change of vWF in the course of treatment.
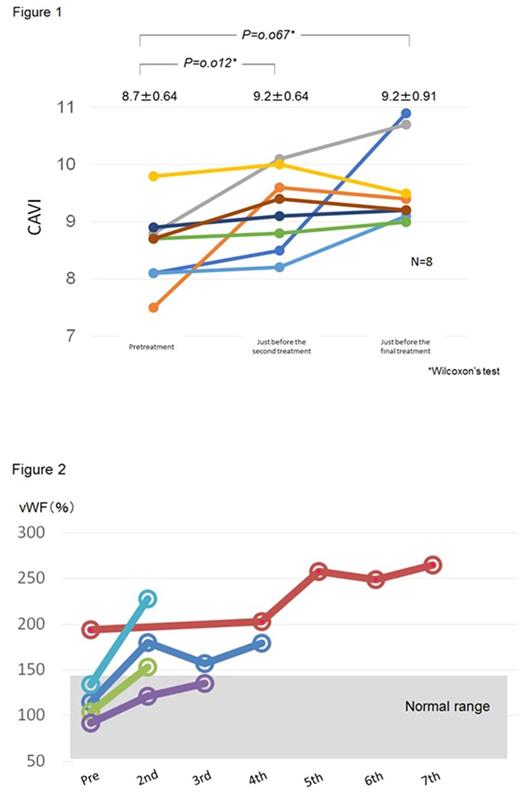
Results: CAVI was evaluated in 8 patients (4 men and 4 women, with a median age of 69 years old). Three patients had DM, one had hypertension and 3 patients had HL in their medical histories. Their primary diseases were; 5 with diffuse large B cell lymphoma, 2 with follicular lymphoma and I with mucosa-associated lymphoid tissue lymphoma. The clinical stages of patients were IIA to IVB. All eight patients achieved complete remission after 4 to 8 courses of chemotherapy. Figure 1 shows the changes of CAVI at pretreatment, just before the second R-CHOP treatment and just before the final treatment. The median value of CAVI was significantly elevated from 8.7±0.64 to 9.2±0.64 after the first course (p=0.012), and was elevated to 9.2±0.91) before the final treatment although not statistically significant (p=0.067). Figure 2 shows the change of vWF during the course of treatment in 5 patients. vWF show a tendency to elevate with following the treatment.
Conclusions: We report that patients with B-cell malignant lymphoma showed the elevated CAVI after R-CHOP even after the first course. We also confirmed an elevation of vWF following the course of treatment. These data suggest that R-CHOP therapy might be a risk factor for the progression of arteriosclerosis in patients with malignant lymphoma.
Figure 1. The change of CAVI pretreatment, just before the second course and before the final treatment in patients with malignant lymphoma treated with R-CHOP.
Figure 2. The increment of vWF in patients with malignant lymphoma treated with R-CHOP therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal